Spotlight on Prostate Cancer
St Vincent's Private Hospital Northside
- Home
- Patient News
- Spotlight on Prostate Cancer
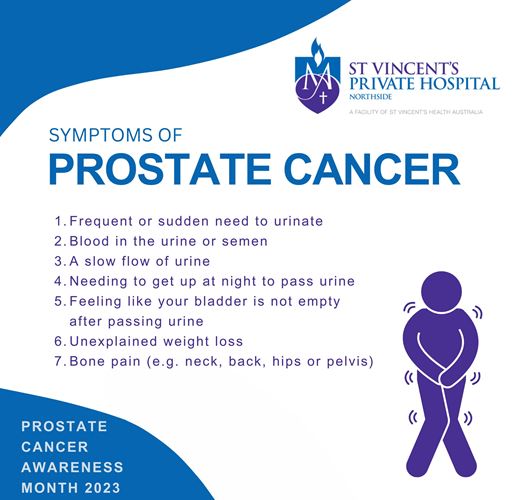
September is Prostate Cancer Awareness Month. The numbers and ages of men being diagnosed are shifting – getting younger. But there is one upside to its rising numbers, say specialists, as it highlights a growing awareness among men and a reduction in the stigma around the ‘awkward conversations’. St Vincent’s Private Hospital Northside puts the spotlight on the issue.
There was a time – not too long ago – when the dreaded ‘P Word’ wouldn’t pass through the lips of men as they sat around chatting at a Friday night barbeque or weekend catchup at the local watering hole. The lips would just sip the beverage!!
But St Vincent’s Private Hospital Northside urological surgeon Dr Jamie Reynolds believes conversations between men about prostate cancer and their own experiences are far more common-place in 2023.
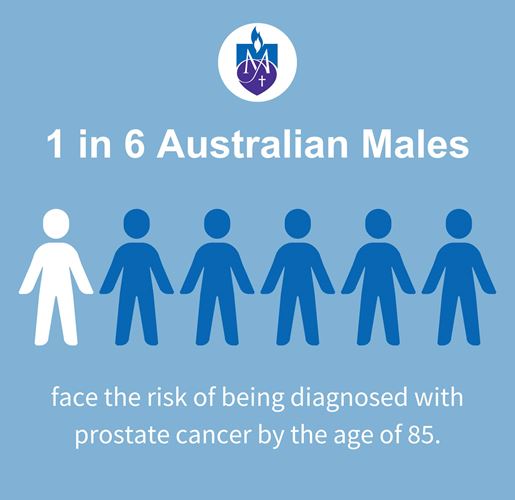
Each year, more than 24,000 men around Australia will be diagnosed with prostate cancer. It’s the second biggest ‘cancer-killer’ of men and is tipped to overtake lung cancer in the coming years, as the number one deadly cancer among males. The average age at diagnosis is 69 years old, while it’s estimated that one in six males will be diagnosed by the time they are 85.
Prostate cancer develops when abnormal cells in the prostate gland grow in an uncontrolled way, forming a malignant tumour.
“Speaking about your prostate isn’t the type of topic or conversation that was easily or comfortably had among men in previous years – there just seemed to be some stigma attached to talking about health issues, especially one such as prostate cancer which can have significant consequences for many men even if detected early,” Dr Reynolds said.
“But it seems as if men are generally more open about it, whether that’s while they’re out on the golf course, at the 19th hole or down at the pub or having a general catch up with mates. They’re not afraid now to say: “How’s your prostate going”? “Who did your surgery? Did you have any complications?” and just generally be prepared to share their experiences and insights.
“Obviously, positive public awareness campaigns such as Movember (the annual event which raises awareness of a range of men’s health issues including prostate cancer) has made a genuine difference in getting the disease into the broader public conversation as well as being a great avenue for fundraising for a variety of projects.”

Dr Jamie Reynolds - Urologist
Dr Reynolds said that the widespread use of robotic surgery for prostate cancer was an important factor in better surgical outcomes with the vast majority of surgery performed using the technology.
"It's minimally invasive surgery using small incisions, and it has benefits over open prostate surgery including less blood loss and need for blood transfusions, and lower infection rates," said Dr Reynolds.
"There's also less pain for the patient, a shorter hospital stay and a quicker return to normal activities."
Fellow urologist at St Vincent’s Private Hospital Northside, Dr David Hussey, said the availability and common use of MRI technology had revolutionised the diagnosis of prostate cancer.
While using the PSA test is a good way for monitoring and detection for prostate cancer, he said, the gold standard and the best way to identify problems is to have an MRI done which provided a reliable diagnostic tool for urologists and patients.

Dr David Hussey - Urologist
“The first step for most men should be to have the PSA test, at least every year, once they reach 55 unless a near relative has been diagnosed or if there is any family history with siblings. Then they should be tested every six months, “said Dr Hussey.
“If the reading is over three, in most cases the GP would recommend a patient get an MRI done and the MRI is a very good way for urologists to get a very clear picture if there are any problems with the prostate gland. If there are potential issues or concerns, then the urologist can opt to do a prostate biopsy which is more invasive.
“The use of MRIs really has revolutionised how we look for prostate cancer. We know that the rates continue to rise as men get older and it’s still true to say that you’re more likely to die ‘with’ prostate cancer rather than ‘from ‘prostate cancer.”
Dr Reynolds performed a robotic radical prostatectomy procedure on Brisbane patient Jim, aged 55 in August 2022. Jim had experienced some issues with ‘his waterworks’ for almost two years – although his access to medical care was constrained with he and his wife being trapped overseas for more than 12 months during the pandemic.
The former Australian Army soldier opted for surgery as he faced the disease, after meeting with Dr Reynolds, believing it offered him the best chance of an optimal health outcome and that decision has been proved right so far.
“I had no family history of prostate cancer and while it’s unclear what triggers cancer sometimes, I have wondered if it was connected in any way to my time in the army when I spent time on overseas postings where I’ve basically been living on top of chemical dumps for months on end and been exposed to who knows what,” said Jim.
“But I also had a great GP, Dr Glynn Kelly of Smart Clinics at Taigum, who worked with me over a period of time in methodically working through the health issues and understanding what was causing them, including have me do PSA tests, ultrasound and an MRI - until we got to the point of doing a biopsy which showed that three of the 12 core biopsy samples were cancerous.
“When I got the cancer diagnosis my wife and I were both understandably very upset – and this was the beginning of a long and painful journey full of questions and doubts. We just wanted to know what were the next steps and how do we tackle this cancer. That’s where our referral to Dr Reynolds was fortuitous.
“He ensured I got lined up for surgery in a timely way at St Vincent’s Private Hospital Northside where the staff and facilities were fantastic. I couldn’t fault it and Dr Reynolds’ should be the ‘poster boy’ for doctor’s bedside manner as he is a terrific surgeon plus he has good communication skills and great empathy.”
Jim has been a regular patient at St Vincent’s over the years with injuries and issues from his time in the Army, notably a back injury which has landed him in the Emergency Department after his prostate surgery.
He says his recovery, while it’s been slow, has been steady and after reaching the ‘first anniversary’ of his surgery he feels as if he’s constantly improving.
Although he does have a message for other men: “We’ve all got a sixth sense about when things just ‘aren’t right’ - whether that’s about our health or in everyday situations. Trust yourself and act on your intuition, it may save your life. I had to put my prostate issues to the back of my mind because we, like many others, were trapped and left stranded overseas, during Covid and we were dealing with our more immediate concerns. I felt that I had little choice but to wait it out until we were granted permission to re-enter the country that I served and love.
“After more than a year, we were able to return to Australia. I am fortunate and it looks promising that my cancer remained (fingers crossed) within the confines of my prostate. So I’d say if something doesn’t feel right with your health, don’t be complacent and if you’re not getting the answers that make you feel comfortable, then keep searching and enquiring. I was lucky – I may have dodged a bullet, but others might not be so lucky if they’re not vigilant.”

Jim and his wife
Dr Reynolds and Dr Hussey say they’re both seeing more younger men being diagnosed with prostate cancer, although the reasons for it aren’t really clear – beyond the heightened awareness among the community and the fact that men are becoming more proactive and vigilant around detection.
This is supported by a recent study by the British Medical Journal which revealed that the global incidence of early-onset cancer increased by 79.1% and the number of early-onset cancer deaths increased by 27.7% between 1990 and 2019.
Karen Walsh is a nurse practitioner at St Vincent’s Private Hospital Northside specialising in the urology ward.
“A cancer diagnosis is very distressing and confronting for anyone but prostate cancer can be even more so for men given the potential impact on their continence and especially sexual function, “said Karen.
She’s been a urology nurse for 30 years and a nurse practitioner at St Vincent’s since 2020. Karen has spoken with hundreds of patients pre- and post-op around a number of the important issues involving prostate surgery – catheter care, incontinence, erectile dysfunction and pelvic floor strength.
“St Vincent’s offers that all-important prostate cancer support service for patients which comes in many forms. Most importantly we are there to talk with patients and to answer any and every question that they have before and after surgery, “Karen said.
“Some men are very chatty and have lots of questions and are happy to talk about their feelings and their fears and insecurities – especially when it comes to sexual function which can be a distressing and challenging consequence of surgery for younger men in their 40s and 50s.”

Karen Walsh - Nurse Practitioner (Urology)