Ryan urges men to see their doctor if something doesn't feel right with their body
St Vincent's Private Hospital Northside
In the realm of the wise adage: “If something doesn’t feel right with your body, see your doctor”, 51-year old Ryan Janes wants men to follow that sage advice and his recent lived experience – and hopes it might help to save their life!
In his case, the 'something’ related to his urinary habits – and a proactive approach to his health led to Ryan and his doctors catching an aggressive prostate cancer just in time before it turned deadly!

“I’ve been lucky to be in good health most of my life. I played a lot of soccer and golf and have always kept active and tried to be health conscious, although when I was younger - like most blokes – I ate and drank what I wanted,” says Ryan, of Brisbane.
“When I hit my 40s the body started to slow down and I started to get regular blood tests just to keep a check on various things. But last year, I noticed that it was getting more difficult when I went to urinate. I’d end up standing there for longer and I just knew something wasn’t right - it wasn’t normal for me.
“It took a couple of trips to the GP and I had to be a bit persistent with the doctor, as they thought I was too young to have major problems with my prostate, being in my 40s. Also my PSA test results fluctuated a bit. “I saw urologist Dr Jamie Reynolds at St Vincent’s Private Hospital Northside and he organised for me to have an MRI then a biopsy.”
The results came back and Ryan heard those fateful words which no one wants to hear: “You’ve got cancer”. His initial reaction was shock but that was quickly followed by a more pragmatic mindset: ‘Right, how we do we fix this? And whatever that involves, let’s deal with it one step at a time.’
“I never really wasted any time or energy asking or trying to find out how or why I got it, there was never any ‘Why me? Or ‘Woe is me’ moments,’ says Ryan.
“Having grown up in country Queensland, I’m a fairly pragmatic sort of person. Also early in my career, I worked for many years as a meat inspector and I would always remember occasionally seeing animals with tumours the size of footballs so that kind of stuck with me.
“When I knew that I had a tumour, it made me realise that I shouldn’t delay at all because I had seen what happens if you let things go for a while and ignore it.
“So when Dr Reynolds recommended that the best option was to remove the prostate gland (in what’s known as a ‘radical prostatectomy’) I didn’t hesitate for too long and agreed to that course of action.”
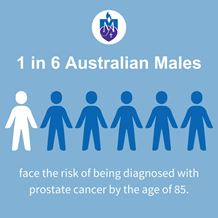
Prostate cancer is the most commonly diagnosed cancer in Australia and the most commonly diagnosed cancer among Australian men.
There has been a surge in the number of cases in the past year, with a record 26,368 Australian men diagnosed with prostate cancer while it’s expected 3,901 men around the nation will die from the disease this year.
However, an even larger tsunami of prostate cancer cases is headed our way – along with the commensurate financial burden to patients, families and the community. Prostate cancer costs more than $1.35 billion to treat every year and accounts for more hospitalisations than any other form of cancer.
And the number of men living with the disease is expected to increase by as much as 50 per cent between now and 2040 – with the Prostate Cancer Foundation of Australia saying the health system could be at risk of crisis if the public and private health systems fail to expand specialist services to support newly diagnosed patients.


Dr Reynolds says patients like Ryan Janes are increasingly common – younger and with minimal symptoms, which in some cases can still mask an aggressive cancer.
“The best course for Ryan was to do the prostatectomy which we did here at St Vincent’s Northside with the Da Vinci robotic surgery,” says Dr Reynolds. “The widespread use of robotic surgery for prostate cancer is an important factor in better surgical outcomes with the majority of surgery performed using the technology.
"It's minimally invasive surgery using small incisions, and it has benefits over open prostate surgery including less blood loss and reduced need for blood transfusions, and lower infection rates. There's also less pain for the patient, a shorter hospital stay and a quicker return to normal activities.”
St Vincent’s Northside has offered robotic technology for surgeons to perform prostatectomies (as well as other general/colorectal surgery) since 2015. Using the Da Vinci system, an advanced robot-utilising technology first developed by NASA, it allows them to remove the prostate gland through small incisions. During the procedure, the da Vinci system translates every hand movement the surgeon makes in real time to bend and rotate the instruments with precision.
St Vincent’s surgeons have performed around 650 robotic procedures since 2015.
From Ryan’s perspective, he couldn’t have been happier and says he got “the best possible outcome” from his surgery with Dr Reynolds.
“Everything works fine just as I want it to and I was thankful that I didn’t need radiation after the surgery,” he says.
“And I’m using my personal experience for the greater good. My brother and brother-in-law have been tested lately and I know there’s a number of guys I work with who have been prompted to go and get their prostate checked out.
“I just tell people – listen to your body, listen to that voice in your head. If it’s telling you that something doesn’t feel right then see your doctor and get things checked out.
“But be persistent about getting to the bottom of the issue even if you’re told ‘you’re too young for cancer or you don’t fit the risk profile’.”
Dr Ben Martin is a leading urologist at St Vincent’s Private Hospital Northside and says he and his colleagues have noticed an increasingly younger cohort of men being diagnosed with prostate cancer over the last decade. But he says the increasing use of MRI and PET scans have been a “significant game changer” in providing early and accurate diagnostic assessment for men with health concerns.

“We’ve known for a while that the PSA test (a blood test performed to assess a man’s risk of having prostate cancer) isn’t perfect and some people say it’s a waste of time because PSA levels can fluctuate.
But by doing the test, it does give patients and their GPs the opportunity to initiate further assessment and awareness with a urologist,” says Dr Martin.
“If there are concerns about the accuracy or results from a PSA, the referral to a urologist who can organise an MRI or PET scans will get to the bottom of the issue. I think men are getting the message about having open dialogues between each other and with their GPs and the critical importance of early detection via testing.
“That awareness is also enhanced by knowing and understanding your family history of prostate cancer. If your father or uncles were diagnosed when they were under 50 there’s a higher risk of prostate cancer for the next generation of men – so knowledge and awareness is power – and could also be a lifesaver.”
- Home
- Patient News
- Ryan urges men to see their doctor if something doesn't feel right with their body